Lyme borreliosis and tick-borne coinfections
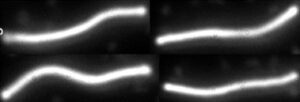
Dark-field image of Borrelia burgdorferi bacteria
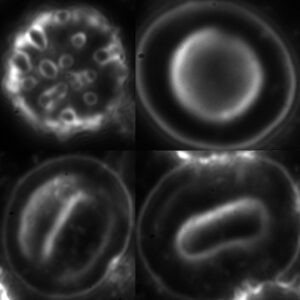
Lyme borreliosis, or Lyme disease, is the most common animal-to-human infection worldwide and the most common tick-borne bacterial disease. The causative agent of the disease is a bacterium called Borrelia burgdorferi: a highly motile, wavy-shaped bacterium classified in the genus Borrelia, a spirochete, which is about 15 micrometers long and 0.2 micrometers wide. It is also called a Teflon parasite because its surface is covered with a special substance, it only has a few surface antigens, so the antibody protecting the host can hardly attach to it. Without treatment, it can hide in the body for years and decades. In addition to its extraordinary adaptation and excellent defensive ability, this is also due to its vegetative forms, the so-called gemmas.

Lyme borreliosis is caused by bacteria that get into the open skin wound caused by a tick bite. Pathogens can vegetate in the middle intestine of ticks for months or years. The tick bite is painless, so bloodsucking can last for days and the blood infected in this way can return to the wound, directly into the small vessels.
Lyme borreliosis can attack any organ months or even years or even decades. This is because the pathogen can reach anywhere with the circulation, and under suitable conditions, if our immunity decreases, it causes an inflammation of a chronic nature. Its spontaneous healing has not been proven, but it can be effectively cured with antibiotics.
According to our current knowledge, the disease does not spread from person to person, it is transmitted from infected animals to humans through ticks. The exception is mother-to-child transmission, which can occur through the placenta and cause infection of the foetus.

Early and diagnostic sign of the infection is the erythema or Lyme rash, which usually looks like a bull’s eye: red inflamed, and intact-looking areas of skin can alternate. However, it may appear differently, more purplish or not always in a bull’s eye pattern. Sometimes it is partly covered for example, under the hair, so it is difficult to determine its shape. The Lyme rash spreads from day to day.
The Lyme rash may not always be present after a definite infection. Only in about one-third of the cases does this type of dermatitis develop, or is noticed by the patient.
Lyme disease often causes chronic dermatitis (atrophy or scarring), but it also damages the nervous system (neuritis, mainly cranial nerves, meningitis, encephalitis), the joint and musculoskeletal system (mainly large joints, but also small joints) and the heart (pericarditis, arrhythmia). In fact, it can affect any of our organs, since it is a disease of the whole organism. Therefore, even if the Lyme rash disappears, it does not mean that Lyme borreliosis has been cured!
Borrelia burgdorferi, the causative agent of Lyme disease, is sensitive to many drugs and can be treated with a variety of antibiotics marketed in Europe. The specialist determines the different types (substrains) of bacteria and their different antibiotic sensitivities and takes them into account when developing the treatment plan. Complete recovery depends on the early detection of the disease, the use of an effective, sufficient, combined antibiotic treatment schedule for the appropriate length of time. A repeated treatment may be necessary. According to our current knowledge, there is no natural or herbal cure that can effectively cure Lyme disease on its own.
Co-infections
Lyme borreliosis is the most common zoonotic disease throughout the world, and also throughout Europe. According to recent statistics, already every fifth person has encountered the pathogen in Central Europe, and one in every seven persons globally. In Europe, there are at least 650-850 thousand new infections per year (according to some estimates, there may be more than 2.5 million). Lyme disease is at least five times more common than AIDS and one and a half times more common than breast cancer. It is becoming more and more common, and this is due to the growing awareness of the disease, but ticks are also gaining ground due to the change in weather patterns. This is because milder weather and no frosts mean more ticks survive the winter. According to some research, infected ticks have a selective advantage in surviving minor frosts.
The bite of a tick can lead to the development of a number of infections. Not only Lyme disease, but also other tick-borne bacterial infections can be spread through the bite. Co-infections associated with Lyme borreliosis and tick bites, Bartonella, Babesia, Anaplasma, Ehrlichia, Mycoplasma and Chlamydia, can cause symptoms similar to Lyme disease. It is very important that tests are carried out to determine exactly whether Lyme disease or one of the co-infections is present so that appropriate treatment can then be started.