Human babesiosis (Babesiosis)
Babesiosis is caused by protozoan parasites living inside red blood cells, which are transmitted by ticks, less often through blood transfusions, or can be transmitted transplacentally to the foetus, i.e. in the womb of the mother.
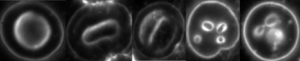
Figure 1. Babesia in red blood cells – with dark-field microscopy
Figure 2. Lifecycle diagram of Babesia
Babesia parasites (and the closely related genus Theileria) are among the most common and widespread blood parasites in the world. Many species of Babesia are capable of infecting humans, Babesia microti is perhaps the most widespread. Infections with Babesia subspecies usually follow a regional distribution; in the United States, cases were mainly caused by B. microti, while in Europe confirmed cases were generally caused by Babesia divergens [1].
Human babesiosis was first detected in Europe in a patient whose spleen had been removed, but most cases have been reported in the northeastern and upper midwestern United States in people with intact spleens and no immune impairment. Cases are reported almost all over the world, Asia, Africa, Australia, Europe and South America. Babesiosis has many clinical features that are similar to malaria and can be fatal, especially in the elderly and immunocompromised patients [2]. Special attention should therefore be paid in cases where Lyme disease has been present for a long time and the persistent presence of Borrelia bacteria has weakened the immune system, making it easier for parasites to spread.
The spectrum of manifestations of the disease is wide, ranging from silent infection to fulminant, malaria-like disease, resulting in severe haemolysis, i.e. breakdown of red blood cells and sometimes death. Babesia infections therefore range from almost asymptomatic to severe. Specific laboratory diagnosis of babesia infection is carried out by morphological examination of blood smears (Giemsa-stained), serology, and – with questionable success – DNA testing (PCR). Babesia infection causes lesions (protrusions and holes) on the surface of red blood cells, and the presence of the pathogen can be visually identified inside red blood cells [1] [3] [4]. The high degree of infection can be identified by simple microscopic examination of the blood, in some confirmed cases the parasite has infected most of the red blood cells [4], while in general cases it is necessary to concentrate infected red blood cells, e.g. by DualDur co-infection preparation method.
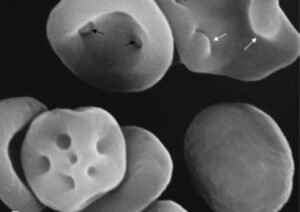
Figure 3. Surface lesions on red blood cells caused by Babesia – electron microscopic image
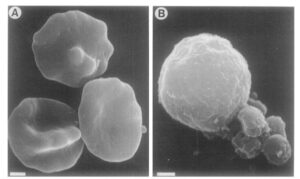
Figure 4. Babesia in red blood cells – electron microscopic image
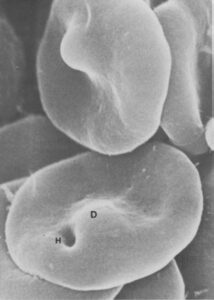
Figure 5. Surface lesions on red blood cells caused by Babesia – electron microscopic image
References
- Homer MJ, Aguilar-Delfin I, Telford SR, Krause PJ, Persing DH. Babesiosis. Clin Microbiol Rev 2000; 13:451–469.
- Vannier EG, Diuk-Wasser MA, Ben Mamoun C, Krause PJ. Infectious Disease Clinics of North America 2015; 29:357–370.
- Braga W, Venasco J, Willard L, Moro MH. Ultrastructure of Babesia WA1 (Apicomplexa: Piroplasma) During Infection of Erythrocytes in a Hamster Model. Journal of Parasitology 2006; 92:1104–1107.
- Sun T, Tenenbaum MJ, Greenspan J, et al. Morphologic and Clinical Observations in Human Infection with Babesia microti. Journal of Infectious Diseases 1983; 148:239–248.